T1D: Disease Overview
For more than two decades, BRI has been a worldwide leader in research to predict, prevent, treat and cure type 1 diabetes. Our scientists have contributed to the identification of diabetes risk genes, the description of diabetes-associated immune cells and the development of laboratory and clinical tools to study disease progression and response to therapy. Our work begins with fundamental laboratory research and extends to clinical trials of new therapies to prevent and treat type 1 diabetes.
What is type 1 diabetes
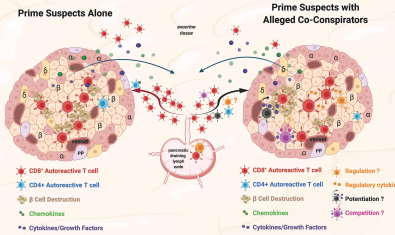
Type 1 diabetes is an autoimmune disease in which the immune system attacks and destroys the beta cells, which are the cells in the pancreas that make insulin, the hormone that controls blood sugar. When there is not enough insulin, the blood sugar rises and symptoms develop, such as excessive thirst, excessive urination, and weight loss.
What causes type 1 diabetes
Type 1 diabetes is caused by a combination of genetic risk and environmental factors that trigger the immune system to attack beta cells. Once the immune attack has started, it continues until symptoms develop and diabetes is diagnosed. Many possible environmental triggers have been considered, and there may be different triggers for different people. Available evidence suggests that diet and other lifestyle factors do not contribute to the development of type 1 diabetes.
What are risk factors for type 1 diabetes?
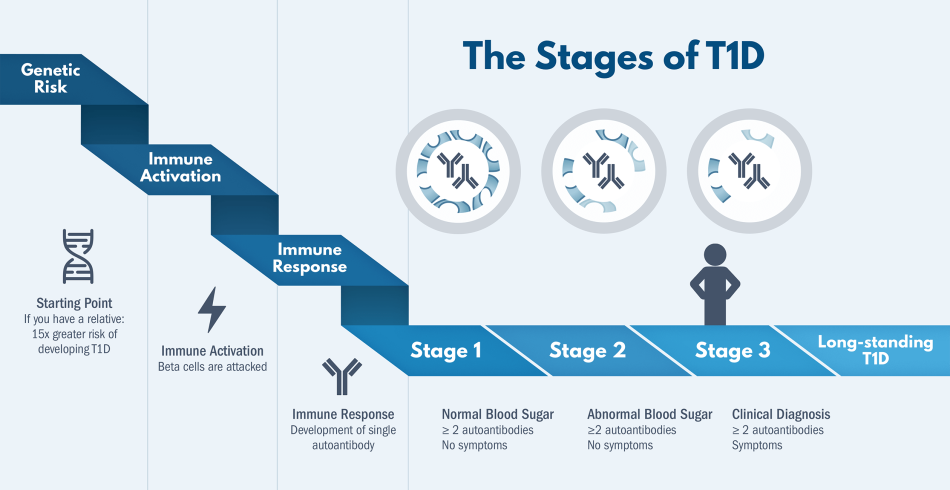
- Having a close family member with T1D. People with parents or siblings who have T1D are 15 times more likely to develop the disease.
- Younger age. About half of T1D is diagnosed before age 18 and about half is diagnosed in adulthood. Most cases of T1D are diagnosed in childhood or the teenage years, although it can start later in life.
- People with Northern European heritage have higher rates of T1D than other ancestry ethnic groups.
Why do people with type 1 diabetes need to take insulin?
People with type 1 diabetes make very little or no insulin so they need insulin to survive. People with type 1 diabetes inject insulin multiple times per day, or use an insulin pump that they instruct to inject insulin. Before eating, they check their blood sugar, count the carbohydrates in the food, consider their activity for the next few hours, and then give insulin. Modern tools like continuous glucose monitors and insulin pumps, which our team helped develop, can make tight blood sugar management easier which reduces the risk of long term complications of high blood sugar including eye, kidney, nerve and heart disease
What’s the difference between type 1 and type 2 diabetes?
While type 1 and type 2 diabetes both affect how the body controls blood sugar, they have different underlying causes and typically require different treatments.
Type 1 diabetes
- Is an autoimmune disease. It happens because immune system cells mistakenly attack the insulin-producing cells. Eventually, this makes the body unable to produce enough insulin to control blood sugar.
- Is typically diagnosed during childhood or young adulthood. About half of people are diagnosed before age 18 and half are diagnosed sometime in adulthood.
- Requires lifelong insulin to control blood sugar levels.
Type 2 diabetes
- Is a metabolic disorder that affects the body's ability to produce and use insulin. It is not an autoimmune disease.
- The pancreas generally produces insulin, but often not enough and it may not be able to use it effectively.
- Is often diagnosed during adulthood.
- Some but not all people with T2D need insulin therapy to control their blood sugar. Others use non-insulin medications or are able to control their blood sugar with lifestyle changes.
What progress has BRI made in type 1 diabetes research?
For more than two decades, BRI has been a world leader in research to predict, prevent, treat and cure type 1 diabetes. Our scientists have made substantial contributions to a future without type 1 diabetes including:
- Identifying specific genes that make a person susceptible to T1D.
- Describing the immune cells that attack insulin-producing cells in T1D
- Developing tools to better understand if and how T1D gets worse over time and how the body responds to different medicines for T1D
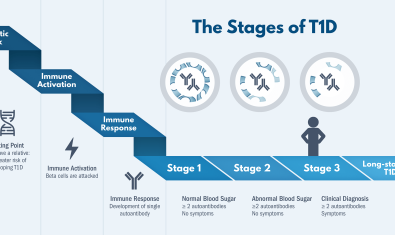
- Supporting research from TrialNet that detailed early immune system changes that predict T1D. These predictors include proteins called antibodies that are present long before a person develops symptoms of T1D. This led to a new staging system for T1D and in 2022, a breakthrough treatment to delay the onset of T1D.
What is the latest research into type 1 diabetes?
Our current research focuses on identifying therapies that modify or support the immune system. Insulin is a lifesaving therapy, but only treats the symptoms of T1D without targeting the underlying cause. Our research aims to:
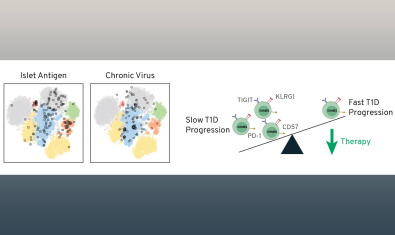
- Find ways to slow or exhaust the cells that attack the beta cells in the pancreas. This could delay the progression of T1D and potentially keep the beta cells working longer. Producing even a small amount of insulin long-term has been shown to lower the risk of complications.
- Prevent T1D. We are seeking therapies that target the immune system changes that happen before a person is diagnosed with T1D, aiming to prevent the disease altogether.
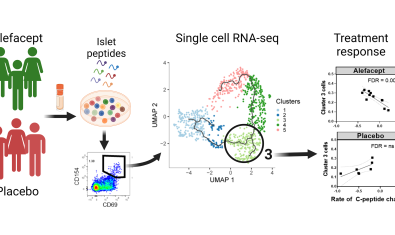
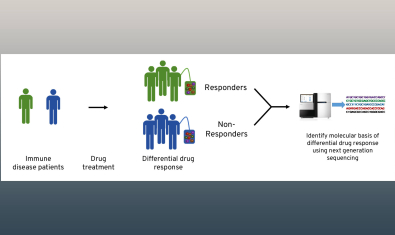
- Find personalized treatments for T1D. No single therapy works the same in every person. We need a library of treatments, with the ability to predict which therapies work best for different individuals. BRI scientists are looking for markers that predict and measure response to different therapies.
BRIAR
The Benaroya Research Institute Autoimmune Registry (BRIAR) is a voluntary registry for individuals interested in participating in autoimmune disease research.
Read MoreBRIDge Study of Type 1 Diabetes
We are inviting you to participate in a research study to help us improve our understanding of diabetes and immune mediated diseases.
Read MoreFABULINUS Study
This study is testing an investigational drug called frexalimab in adolescents and adults age 12-35 years old with newly diagnosed type 1 diabetes who are on insulin therapy (adults age 18-35 will be enrolled first, followed by 12 to 21-year-olds later in the study).
Read MoreIDAD Study
Benaroya Research Institute and the Immune Drivers of Autoimmune Disease Program are conducting a study to understand how the immune system functions differently in people with and without Down syndrome and with and without diabetes risk markers.
Read More
Labs studying type 1 diabetes
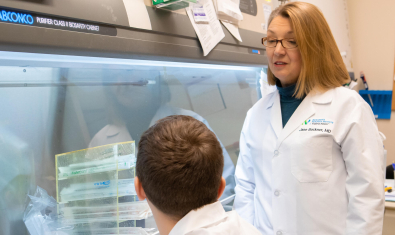
Buckner Lab
The Buckner Lab is focused on identifying the underlying mechanisms by which regulation of the adaptive immune response fails or is overcome in the setting of human autoimmunity.
Campbell Lab
The Campbell laboratory is interested in understanding the basis for T cell activation, function and tolerance.
Cerosaletti Lab
Dr. Cerosaletti’s research is focused on the role of the adaptive immune system in the development and progression of immune mediated diseases and the response to treatment.
Greenbaum Lab
Our group focuses on prediction and prevention of type 1 diabetes (T1D) as well as discovery and validation of biomarkers of disease progression and response to therapy.
James Lab
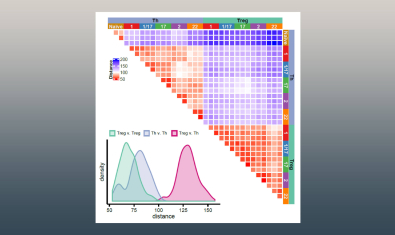
The James lab is working to develop an increasingly in depth knowledge of autoreactive T cell responses by examining the characteristics of the epitope specific cells involved in autoimmune diseases through robust multi-parameter assays and also at the single cell level.
Kwok Lab
The Kwok lab uses tetramers and other antigen specific T cell assays to examine autoreactive T cells in autoimmune diseases in order to provide insights into disease mechanisms and identify strategies for disease intervention.
Linsley Lab
Our goal is to develop and use cutting edge systems biology approaches to elucidate molecular signatures of complex immune diseases, understand the mechanisms of disease, and identify the right therapy for the right patient.
Long Lab
The Long Lab focuses on understanding mechanisms of tolerance, why they are lost in autoimmunity, and how tolerance can be augmented with therapy.
Speake Lab
The Speake group is interested in advancing clinical research – especially in type 1 diabetes, but also in the context of other immune-mediated diseases.