In a recent letter in the Journal of Allergy and Clinical Immunology, researchers from Benaroya Research Institute (BRI), Children's Hospital of Philadelphia (CHOP), and Massachusetts General Hospital (MGH) identified the first food antigen-specific T cell from a patient with milk allergy who developed milk-triggered eosinophilic esophagitis (EoE). The results from this study provide additional evidence that EoE is mediated by food antigen-specific T cells.
EoE is a disease that affects both children and adults and is triggered when a patient ingests an allergenic food. It is accompanied by an increase in eosinophils, a type of immune cell that often plays a role in allergic responses, as well as T cells in the esophagus. The immune cell invasion of the esophagus results in inflammation, tissue damage, and fibrosis, which can cause difficulty swallowing, esophageal obstruction, and esophageal dysfunction. Traditionally, EoE has been managed in the clinic as a food allergy, with treatment revolving around dietary avoidance of food triggers. However, this is the first time that a food antigen-specific T cell has been identified in an EoE patient.
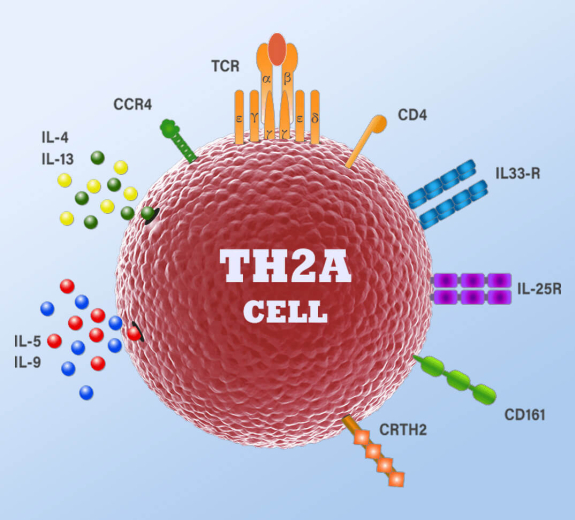
Because of their expertise in single cell RNA-sequencing and T cell receptor (TCR) analysis, Drs. Karen Cerosaletti and Alex Hu at BRI collaborated with the researchers at CHOP who had collected genomic data from T cells from the blood of a patient with confirmed EoE milk allergy. Upon analyzing these data, they identified a milk-specific TCR in the population of pathogenic T helper 2 (TH2) cells, a T cell subset previously observed in the esophageal tissue of EoE patients. They also found that these milk-specific TH2 cells had elevated expression of genes related to activation, cytotoxicity, exhaustion, and regulation, as well as increased interferon signaling. Altogether, this evidence links the detection of milk antigen by an antigen-specific T cell to eosinophilic recruitment, allergic response, and inflammation in EoE.
“With the data that their colleagues collected from an EoE milk allergy patient, Drs. Cerosaletti and Hu we were able to confirm that this case of EoE was mediated by T cell recognition of milk antigen,” said BRI President, Dr. Jane Buckner. “Food antigen triggers likely exist for many patients with EoE. This study lays out an approach for the investigation of these other food allergies in EoE, for which we have little knowledge.”
For more information about BRI, visit BenaroyaResearch.org.