
Weathering Uncertainty with Resilience
Read Article
From Bootstrap Operation to Nobel Prize
Learn the backstory of a discovery that changed our understanding of the immune system and earned a Nobel Prize from Steven Ziegler, PhD.
Understanding the Immune System’s Brakes
Explore work from Daniel Campbell, PhD, examining how a cytokine called IL2 could lead to new therapies for autoimmune diseases.

A Decades-Long Dream Becomes Reality
Learn how research led by Jane Buckner, MD, is bringing regulatory T cell-based therapies closer to clinical trials.
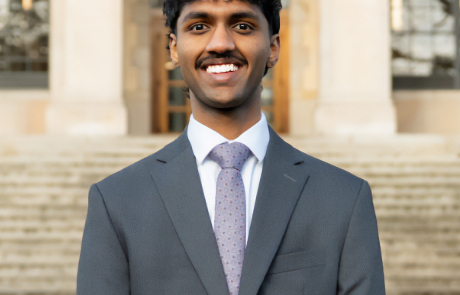
“Keep Asking the Next Question:” Lessons Rhodes Scholar Shubham Bansal Learned at BRI
Learn more about how his time at BRI helped shape 2025 Rhodes Scholar Shubham Bansal.
Mapping Immune Cells in the Skin
Learn how Peter Morawski, PhD, and Hannah DeBerg, PhD, are mapping immune cells in the skin to better understand how they may fight — or fuel — disease.

Innovation Fund Backs Exciting New Research
Allyson Byrd, PhD, and Cate Speake, PhD, are exploring an innovative tool in immunology research. The questions they can ask are limitless.
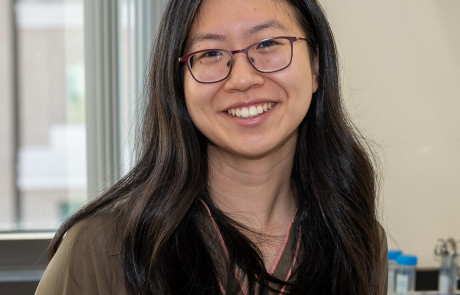
Early-Career Scientist Lucy Li Advances Lupus Research at BRI
Early-career scientists play a vital role in BRI’s work. Meet Lucy Li, who is working to answer pressing questions about lupus as part of her MD–PhD program.
Innovation Fund Spotlight: Exploring Immune System Cells and Gut Bacteria
Allyson Byrd, PhD, is an expert in the gut microbiome, the study of the tiny organisms that live inside our digestive system. James Lord, MD, PhD, is a gastroenterologist who has studied inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis for more than 20 years.
Innovation Fund Spotlight: State-of-the-Art Genome Editing To Understand Disease and Develop New Therapies
Learn how CRISPR-Cas9-based genome engineering using adeno-associated virus (AAV) vectors is helping BRI scientists make breakthroughs to study human T cells and explore new treatments for type 1 diabetes, as well as develop preclinical models to study T cells and B cell
Finding the Root Cause of Lupus
For more than 20 years, Steven Ziegler, PhD, has wondered if an altered version of a protein might play a key role in autoimmune diseases. Now, he finally has the tools to investigate further – and his work could lead to key insights about how and why lupus happens.


