“Even then, immune cells may attack the new liver and the disease can come back,” says Ritika Tewari, PhD. “That’s why finding better treatment strategies is so important.”
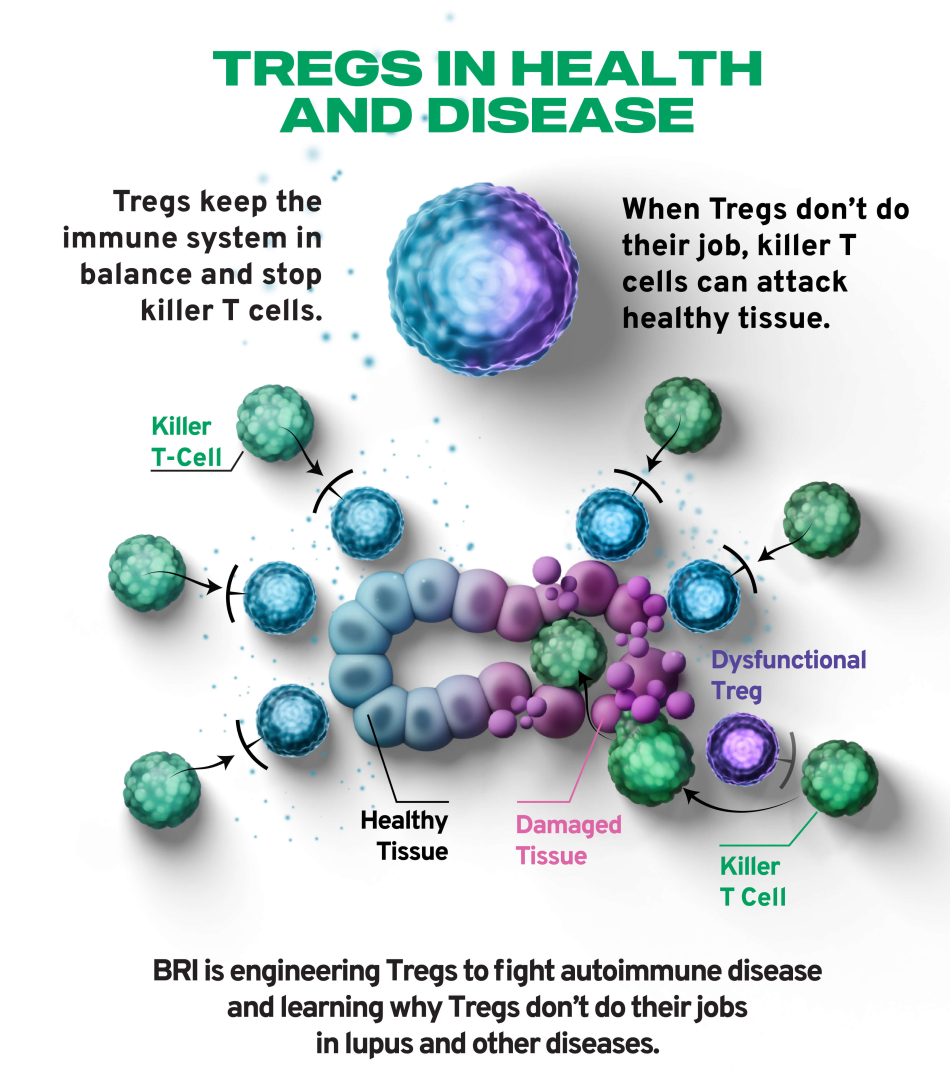
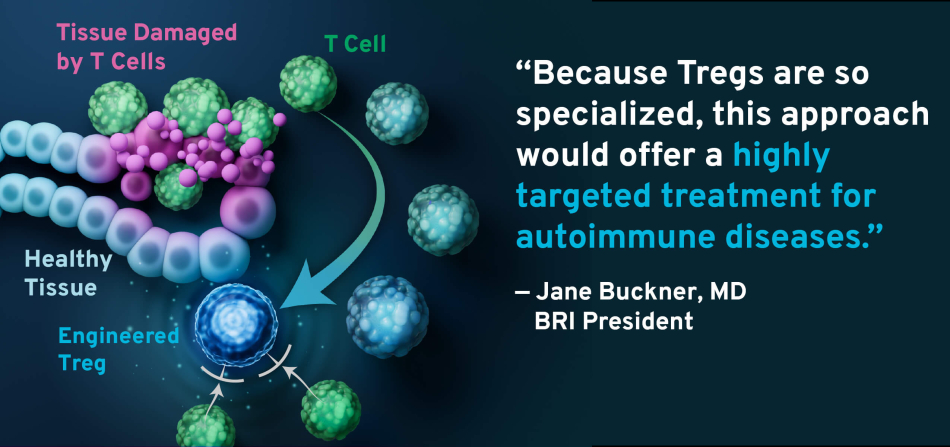
Dr. Tewari and BRI’s Soo Jung Yang, PhD, recently published findings that could pave the way to better autoimmune disease treatment options. Their work focuses on a new approach that BRI’s Buckner Lab is pioneering: turning T cells that contribute to autoimmune diseases into regulatory T cells (Tregs, pronounced “tee-regs”) that help prevent autoimmune diseases.
“This is an exciting advance because our goal is to apply this approach to many different autoimmune diseases — whether common or rare — in hopes of offering a more targeted and effective treatment,” Dr. Tewari says.