Gut Immunity Program
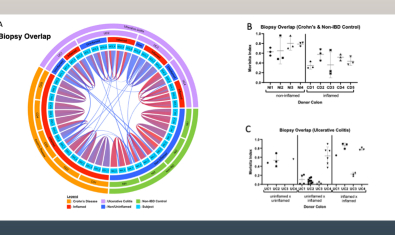
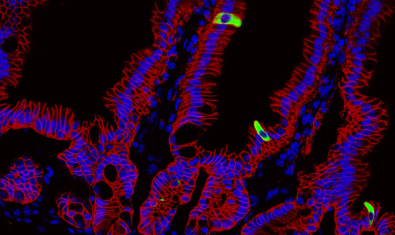
The Gut Immunity Program at Benaroya Research Institute studies how immune responses in the gut go wrong and lead to inflammatory bowel diseases (IBD) such as, celiac disease, Crohn's & colitis and other autoimmune conditions. Researchers use model systems, biorepository samples and clinical studies to understand how immune responses go awry. They also study the gut microbiome and how immune responses in the gut contribute to other autoimmune diseases.
Established in 2019 with the support of a $3 million donation from a private donor, this program brings BRI closer to understanding what triggers IBD. It also provides researchers with resources to identify new treatments by fostering collaboration and developing new research methods that can then be applied to other immune-mediated conditions. BRI’s expansive resource of cell samples and clinical research partnership with Virginia Mason leaves the institute well positioned for research involving gut immunity.
About Gut Immunity
Ulcerative colitis and Crohn’s Disease are chronic inflammatory immune-mediated diseases. 1.6 million people in the U.S. have IBD and the numbers are increasing. While some some treatments exist, there are no known preventions or cures. These diseases are thought to be influenced by several factors, including the immune system, gut microbes and lifestyle/environment.
Additionally, gut immunity is believed to play an important role in whole body immunity such that the health of the gut may impact other organs, including the skin and lungs.

Labs in the Gut Immology Group
These are the labs that make up the gut immonology program.
Harrison Lab
Lacy-Hulbert Lab