Connecting Immunology Research to Cancer Treatment
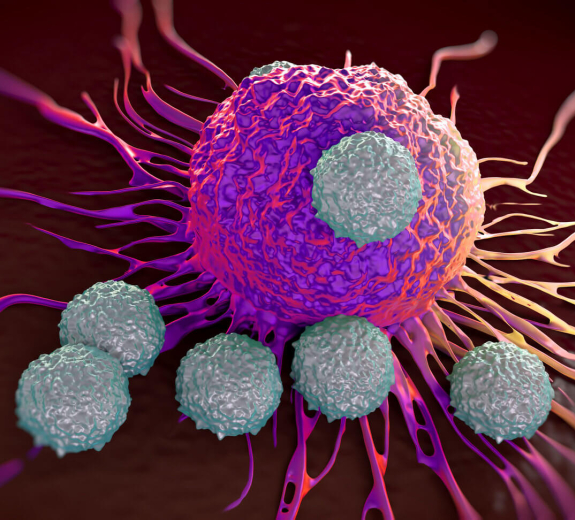
BRI has been active in tumor immunology research since the 1970s — back when the institute was still called Virginia Mason Research Center. Since that time BRI has been involved in clinical trials at Virginia Mason, investigating immunotherapies for cancer treatment as well as basic research focused on understanding how aspects of the immune system might be harnessed to fight cancer.
Applying Immunotherapy to Urologic Cancers
Through participation in clinical trials, BRI’s Clinical Research Program is on the cutting edge of cancer immunotherapy research. Over the past 10 years, John Corman, MD, Medical Director of the Floyd & Delores Jones Cancer Institute at Virginia Mason and BRI board member, has been a site investigator for many clinical trials, one of which led to the FDA approval of Provenge to treat advanced prostate cancer. Provenge is a personalized therapy in which a patient’s immune cells are activated against prostate cancer in the laboratory, and then infused back into the patient. It is the first FDA-approved treatment of its type and the only FDA approved immunotherapy for advanced prostate cancer. Follow-up studies to the Provenge trial are investigating Provenge in combination with other agents. A trial, which is currently recruiting patients, is investigating a different immunotherapy that utilizes immune cells activated against prostate cancer, DCVAC/PCa, in combination with standard chemotherapy. Another, which recently completed enrollment, is investigating a novel vaccine approach to metastatic prostate cancer called PROSTVAC.
TSLP: Allergic Diseases to Cancer
Current research in the laboratory of Steven Ziegler, PhD, funded in part by the National Cancer Institute, is investigating the role of thymic stromal lymphopoietin (TSLP) in the growth and metastasis of tumors. TSLP is a cytokine that the lab has been studying in relation to the development of asthma and other allergic diseases. It is normally expressed in epithelial cells at barrier surfaces in the lungs, skin and gut. When it was shown that increased TSLP is found in breast and pancreatic tumors, and that increased levels are correlated with negative patient outcome, the laboratory began investigating TSLP in cancer models. The lab has shown that TSLP is critical for both tumor growth and metastasis. Using model systems of metastatic breast cancer, they have demonstrated that the primary tumor is reduced in size by 80% and metastasis to the lung is dramatically reduced in the absence of TSLP. The same impact is seen with an anti-TSLP antibody that is similar to an antibody currently in phase two clinical trials for the treatment of asthma. The lab is hopeful that their findings will result in a clinical trial for anti-TSLP antibody in the treatment of breast cancer.
Using Module Analysis to Predict Treatment Outcome
Recent work in the lab of Peter Linsley, PhD, has been investigating immune modules, co-regulated immune gene expression levels, in solid tumors. In an initial study published in PLOS ONE in October 2014, Linsley analyzed immune modules for their ability to predict melanoma patient survival. The project utilized data from the Skin Cutaneous Melanoma (SKCM) dataset from The Cancer Genome Atlas (TCGA). He demonstrated that increased expression of type 1 interferon-stimulated genes (ISGs), T helper/T regulatory and NK/T cytotoxic cell genes significantly predicted patient survival. Current work in the Linsley lab is expanding the module analysis of immune gene expression levels to 11 other different tumor types to identify genes that are both positively and negatively correlated with patient survival.


