Endemic vs epidemic vs pandemic: What is an endemic disease?
When a disease is endemic, it is always present in a certain area or population. The number of cases that happen each year is generally stable.
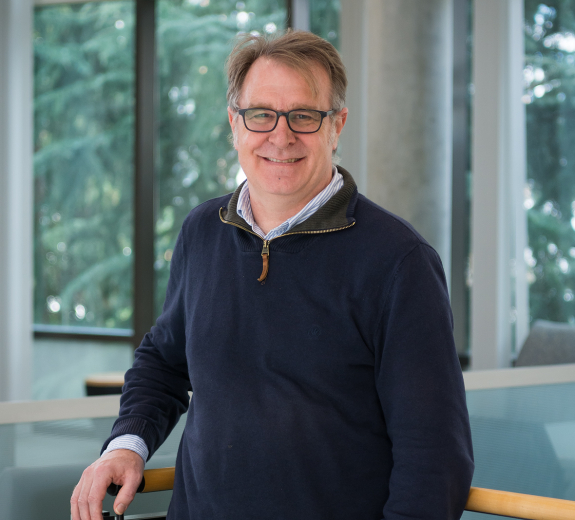
“With endemic diseases, you don’t really see these huge explosions of cases going up and up like we have during the COVID pandemic,” Dr. Lacy-Hulbert says. “Generally, we have a good idea of how much it will spread and when it will stop.”
Here’s how endemic diseases are different from epidemics or pandemics:
-
Endemic: A disease that is always present at some level and relatively predictable in how and when it will spread. For example, the flu is considered endemic in the United States.
-
Epidemic: An epidemic is when cases of a certain disease start rapidly increasing in a specific area or among a certain population. For example, the Ebola epidemic in West Africa between 2014 and 2016. There was a rapid, unpredictable increase in cases but it was generally contained to one geographic area.
-
Pandemic: A pandemic, like COVID-19, happens when a disease spreads at unpredictable levels globally.
Are endemic diseases less dangerous? What are some examples of Endemic diseases?
“Endemic doesn’t mean ‘not dangerous,’ it's more a measure of how established a disease is,” Dr. Lacy-Hulbert says. “For example, HIV is considered endemic in some areas. But HIV without treatment is deadly. So endemic diseases can still pose a threat, particularly if you don’t have vaccines or treatments for them.”
Different parts of the world have different endemic diseases. Malaria is considered endemic in areas like Sub-Saharan Africa and South Asia. While healthcare providers have many tools to prevent and treat malaria, the World Health Organization reported 241 million cases and estimated 627,000 deaths from the disease in 2020.
Other endemic diseases are less deadly.
“The common cold is endemic,” Dr. Lacy-Hulbert says. “You might have a time in the winter where suddenly everyone you know seems to have a cold, and other times you can't remember having a cold for months. So, ‘endemic’ doesn't mean that you’re sick all the time. But it’s always around, there's always a chance to get a cold.”
How does COVID-19 moving toward endemic change research surrounding the virus?
As COVID-19 continues to be part of life, virus researchers will continue to examine what new variants might look like, including if and how they might affect people — and if vaccines will continue to protect us.
Researchers at BRI will continue to focus on questions about how COVID-19 impacts the immune system and how we can maintain protection moving forward. For example, Erik Wambre, PhD, is zeroing in on how long protection from COVID-19 vaccines last. Carmen Mikacenic, MD, is working to understand how and why people get long COVID, and best practices for treating people experiencing lasting symptoms from the virus.
What does endemic COVID-19 mean for people who are immunocompromised?
The last thing that people who are immunocompromised want to hear is that COVID-19 will be around forever. Researchers at BRI and beyond are working to understand exactly how certain immune system diseases (and the medicines you take to treat them) impact how vaccines protect you. This includes ongoing COVID-19 vaccine studies among people with multiple sclerosis, rheumatoid arthritis, inflammatory bowel disease and Down syndrome.
Scientists are also working to develop ways to protect people who do not have as strong of a response to vaccines, such as:
- Passive immunization, where people can receive a preventative shot of virus-fighting antibodies that can help protect them if they’re exposed to the virus.
- New therapies to treat COVID-19 that can be given right away to reduce their risk of complications.
“We can’t expect people who are immunocompromised to stay at home forever,” Dr. Lacy-Hulbert says. “The hope is that antibody shots and new treatments will provide better options, while enough of the rest of the population will have been vaccinated and/or exposed which will increase immunity and reduce how much the virus spreads.”
Pandemic to endemic COVID: How do we stay safe in the next phases of COVID-19?
After years of living with COVID-19 restrictions in place, the idea of attending large gatherings or going anywhere without a mask might seem daunting. As restrictions roll back, how do we know if it's really safe?
Dr. Lacy-Hulbert recommends following your local public health guidelines. Keeping an eye on case numbers and number of hospitalizations in your area can provide more insight into how prevalent the virus is in your community.
Moving forward, we can expect some measures to be in place for the long-haul, like vaccination and staying home while you’re sick. Other regulations may be lifted when case numbers are low, and reinstated when case numbers are high.
“Everyone should get vaccinated and be prepared to get another booster shot if it is recommended, even if case levels are low at that time. That’s the thing about endemic diseases — they come back,” Dr. Lacy-Hulbert says. “And when another outbreak happens, we should be prepared to do things like put on our masks and limit the size of events to reduce spread.”
Considering your own personal risk and the risk of those around you will continue to be important moving forward.
“Some people will want to continue to wear masks when restrictions are lifted and that’s perfectly okay,” Dr. Lacy-Hulbert says. “One thing to consider is if you or anyone who you are in close contact with might be at high risk for complications — who might you expose?”
COVID-19 will likely become endemic…in the northern hemisphere?
In talk of endemic COVID-19, there’s a caveat: It’s largely becoming endemic only in the northern hemisphere, at least for now. While the virus is becoming more predictable in the United States, that’s not the case for many other countries.
“We need to turn our attention to bringing vaccines and access to treatments to the rest of the world,” Dr. Lacy-Hulbert says. “People everywhere should have the same access to the treatments and vaccines we have here. This is important both from a human rights perspective and from the perspective of controlling the disease. The more infections you have, the more mutations you have and the more likely new variants are to arise.”