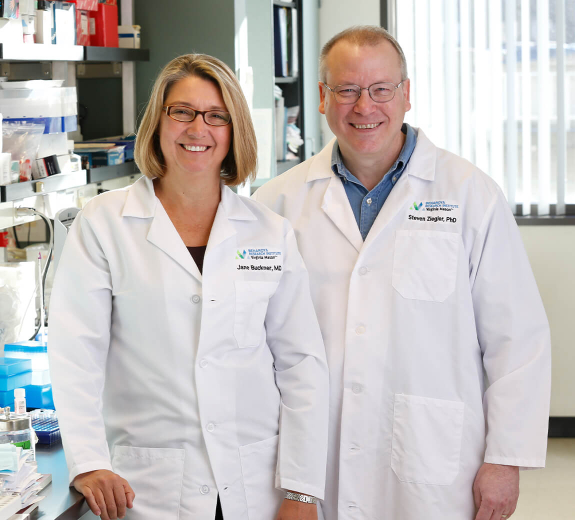
“We’re moving closer to the first human trials using this approach,” Dr. Buckner says. “And it could shift the paradigm of how we treat autoimmune disease.”
FOXP3 Sheds Light on Autoimmunity
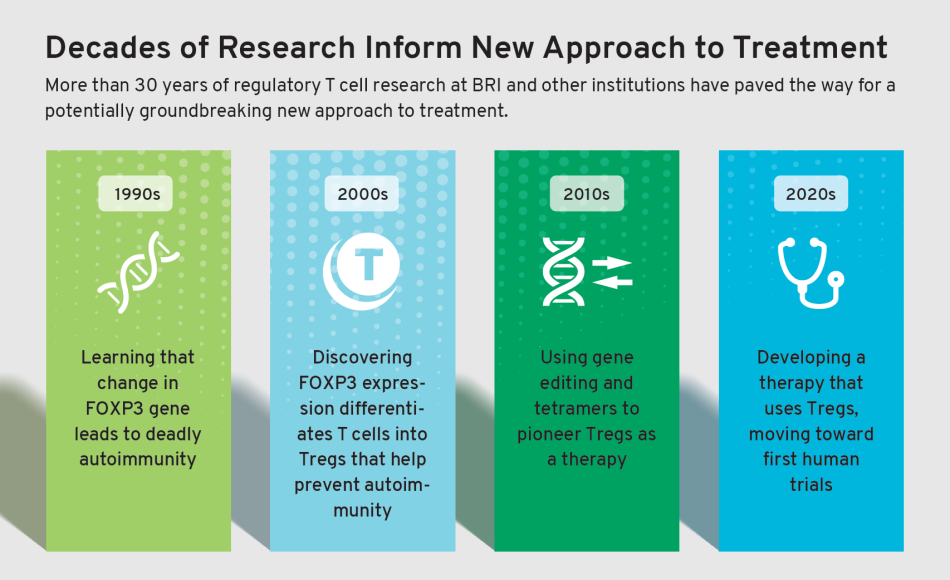
BRI’s Steven Ziegler, PhD, was involved with research in the early 2000s that put this new approach in motion. He learned that a single change in a gene called FOXP3 triggered fatal autoimmunity in lab experiments. Shortly after, he learned that the very same gene was involved in a similar disease that could lead young children to die from autoimmunity.
“Scientists at Seattle Children’s and Washington University in St. Louis found that those kids had mutations in the same gene we saw in the lab,” Dr. Ziegler says. “That showed the power this gene has in the immune system: loss of function leads to deadly autoimmunity.”
If changing FOXP3 ever so slightly means severe autoimmunity, Dr. Ziegler reasoned that the same gene must protect the body from autoimmune disease when it’s working properly. He and other scientists set out to learn more.
The sum total of their findings shifted scientists’ entire understanding of autoimmune disease. They learned that FOXP3 is required for regulatory T cells (Tregs, pronounced “tee-regs”) — a rare cell type that helps protect against autoimmune disease.
What are Tregs?
Tregs are a type of T cell. T cells are supposed to protect your body by attacking invaders like viruses and bacteria. But in autoimmune disease, they mistakenly attack healthy tissue.
Tregs, on the other hand, are supposed to act as quality control, ensuring all other T cells are doing their job — attacking invaders and not healthy tissue. Tregs are also highly specialized: Some solely protect the pancreas from diabetes, while others protect joints from rheumatoid arthritis (RA).
Discovering Tregs was a huge breakthrough that led to a key question: Could scientists harness their power to create a highly targeted new treatment for autoimmune disease? But there was a catch.
“Unfortunately, Tregs are incredibly rare and hard to find,” Dr. Buckner says.
Luckily, BRI had just the tool to find a needle in a haystack: tetramer technology, developed by BRI’s Bill Kwok, PhD, and Jerry Nepom, MD, PhD, which allows scientists to find a few specific cells among millions.
Highly Targeted Treatment
Since the development of tetramer technology, BRI investigators have become experts on identifying cells that target healthy tissue and promote autoimmunity. BRI investigators wanted to examine those cells and use them as a roadmap to create Tregs — to target disease-causing cells and stop autoimmunity.
A similar approach is already being used in immunotherapies that target cancer. These therapies reprogram a person’s cells to attack cancer cells, making them more precise and potentially less harmful than radiation and chemotherapy.
“We want to use a similar principle for autoimmune disease: Turn attacker cells into Tregs so they stop attacking,” Dr. Buckner says. “And because Tregs are so specialized, this would offer a highly targeted treatment. If T cells are attacking the joints, we can reprogram those cells to protect the joints from RA. This new treatment would only affect disease-causing cells, not the whole immune system.”
As BRI’s team worked toward this goal, they hit another roadblock: They needed to ensure that if they turn attacker T cells into Tregs, they never turn back into attacker cells.
“This was tough and we started to lose hope,” Dr. Buckner says. “Then CRISPR, a new gene editing tool, came online. That changed everything.”
Teamwork Fuels Progress
When this tool came online, BRI partnered with David Rawlings, MD, and his team of gene editing experts at Seattle Children’s Research Institute. Together, they found a way to make any T cell a Treg and keep it that way forever.
Following additional lab studies, Drs. Buckner and Rawlings helped found a company called GentiBio in 2020. GentiBio’s goal is to pioneer new medicines that use this approach, and they’re rapidly developing an engineered Treg as a therapy for type 1 diabetes. Then they’ll apply it to other autoimmune diseases, allergic diseases and transplant recipients.
This approach still has a long way to go. But it signals immense potential progress toward more targeted therapies with fewer side effects.
“Advances like this aren’t the work of any individual — they’re the effort of many scientists,” Dr. Buckner says. “It’s the physicians and patients who donate samples and donors who support our work. With all of these people on our side, BRI’s vision feels within reach: a healthy immune system for everyone.”
Philanthropy Powers Possibilities at BRI
Dr. Buckner and Dr. Rawlings of Seattle Children’s teamed up to advance this research, which was fueled by a generous $4 million grant from the Leona M. and Harry B. Helmsley Charitable Trust. Foundation grants and philanthropy fuel BRI’s research by supporting innovative ideas and helping scientists collect preliminary data needed to apply for larger government grants.