An Unprecedented Way To Study Rheumatoid Arthritis
The first symptoms Linda Sloate experienced were aching hands and pain that shot up her arms. She had carpal tunnel surgery in both hands. Then she felt pain in her feet while she was teaching kindergarten and running around after her three children.
“I was diagnosed with rheumatoid arthritis (RA) and I said ‘Huh? I’m 30.’ I thought only older people got RA,” Linda says. “RA is a battle. Your whole body feels achy, destroyed. Sometimes every bit of you hurts from the top of your head down to your toes.”
She started seeing rheumatologist Jeffrey Carlin, MD, who was eventually able to enroll her in a trial of a then-new therapy — etanercept (sold under the brand name Enbrel). Linda still remembers the morning after starting the medication.
“I woke up and felt normal, the way I was supposed to feel,” she says. “I just looked up to God and said, ‘Thank you.’ Then I brought Dr. Carlin flowers and a latte."
Linda has been on that therapy for decades and it's helped her live with less pain. But RA has still taken a toll: She can only use three fingers on each hand. She’d had numerous hand surgeries and multiple foot surgeries. And when she couldn't bend her arms to hug her grandkids, she had two elbow replacements.
Most recently, she had a knee replacement — and opted to donate her tissue to a BRI study led by Eddie James, PhD. His team is studying tissue samples to gain unprecedented insight into how and why RA happens. The goal is to inform treatments that target RA at the source, slowing long-term joint damage and reducing symptoms.
Attacker T cells and attacked proteins
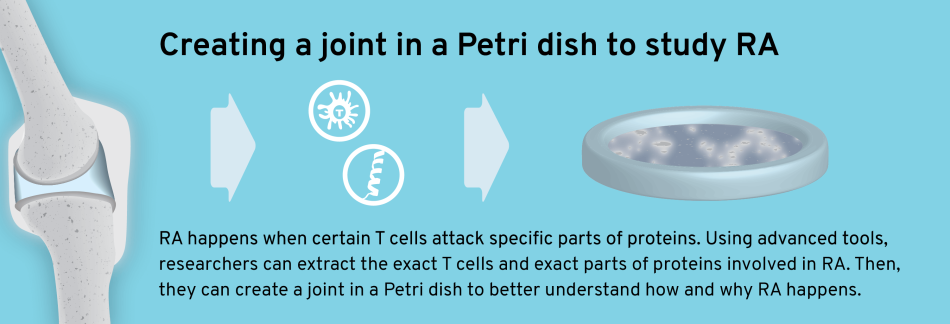
RA happens when immune cells called T cells mistakenly attack proteins in the joint. Scientists are typically only about to study immune cells from blood to learn more about how and why this happens. But thanks to participants like Linda, our team is among the first to study the T cells from joint tissue to identify the exact proteins involved in RA.
The researchers aim to answer two questions: What causes certain T cells to attack? And which peptides (small fragments of proteins) are they attacking?
They’re studying attacker T cells in precise detail — cataloging thousands of peptides, working to pinpoint which ones are recognized and attacked in RA. Then, researchers will re-create a joint in a Petri dish, putting the T cells and proteins together to confirm how cells attack and which peptides are being attacked.
“This would give us ironclad evidence that specific T cells attacking a specific peptide sequence is central to the disease,” Dr. James says.
Targeting RA at the source
Down the road, this research could inform game-changing RA treatments — like antigen-specific therapies, which teach your immune cells to stop attacking.
“If you know which peptide is being attacked, you can teach the body to ‘tolerate’ it and stop attacking,” Dr. James says. “That could reduce the intensity of disease or move patients into remission.”
Knowing more about attacker cells could also inform better therapies that use “designer regulatory T cells” to slow down the attack.
“Once we know which peptide a T cell recognizes, we can basically fish that cell out and create an artificial version of that cell that responds to the same peptide but has the opposite effect: It suppresses the immune response that’s hurting the joints,” Dr. James says.
New research, new hope
The research team is just over one year into this four-year project, and they’ve already collected some key data. If their approach proves effective in RA, it could also provide insight into other autoimmune diseases like multiple sclerosis.
As for Linda, she’s now retired and enjoys sewing and spending time with her family. She does everything she can to support RA research.
“Who would ever think your cells would be famous?” Linda says. “All of this research and new tools are so wonderful. I think back to the famous artist Auguste Renoir in 1892, who developed debilitating RA, and I feel lucky to live in this time with all of the scientific research.
You have to have a positive outlook with this disease RA. When I was diagnosed 30 years ago, it was really isolating — they didn’t know much about RA, there weren’t many people to talk to. But this work leads to new treatments and new hope, and it's just so much better.”
More clues into what causes RA
Jing Song, MD, PhD, is a postdoctoral researcher whose pursuit of immunology has taken her around the world: She did her MD in China, then her PhD in Israel.
“After my PhD, I wanted to continue to do translational research, working in immunology and autoimmunity,” she says. “BRI has this great sample repository and tetramer technology. And Dr. Buckner and Dr. James are just really good at this research.”
She joined the Buckner Lab in 2016 and recently made a key finding. She built on research from Oxford’s Kim Midwood, PhD, who identified a protein that plays a pivotal role in rheumatoid arthritis — and collaborated with Dr. Vivianne Malmström, from the Karolinska Institute, in Stockholm, Sweden.
Dr. Song’s team took a closer look at the cells that attack this protein. They examined small fragments of this protein and found that two types of immune cells, T cells and B cells, were launching an attack. In patients who smoked or had a genetic risk factor for RA, this immune system response was even stronger. Their findings were published in JCI Insight.
“This is the first study which shows T cells and B cells are recognizing the exact same peptides in RA,” Dr. Song says. “This raises the possibility that these cells are basically working together to attack your body, causing RA to develop and get worse over time. This teaches us more about what causes the disease and could open new potential pathways for treatment.”
Immuno-what? Hear the latest from BRI
Keep up to date on our latest research, new clinical trials and exciting publications.


