“Research from our team and many other scientists pinpointed how to predict T1D,” Dr. Greenbaum says. “We also learned that the age you develop T1D impacts disease course and that the pancreas continues to produce a little bit of insulin after diagnosis.”
Better understanding the disease’s course led to another question: How can we change it? Over the years, BRI, TrialNet and other T1D leaders developed therapies that aim to preserve insulin function. This could help maintain some insulin production for people already diagnosed with T1D and possibly prevent the disease.
“Now there are seven therapies that help preserve insulin production after diagnosis and we’re working to see if they can contribute to prevention,” Dr. Greenbaum says. “In 2019, we made a key breakthrough with a trial of teplizumab, which delayed T1D for a median of two years. This is the first therapy to delay any autoimmune disease, and it’s a vanguard of what we anticipate will be many clinical options.”
Moving forward, BRI’s team aims to expand T1D screening and make T1D care more personalized, so each patient gets the best treatment for their unique biology.
“People with T1D are living longer with fewer complications than ever, which is incredible. But it’s not good enough,” Dr. Greenbaum says. “At BRI, we’ve built a culture of creative thinking and a team who see stopping T1D not just as a job but as a mission. And we use that approach to move close to our goal: Predict, prevent, reverse and cure T1D and all immune system diseases.”
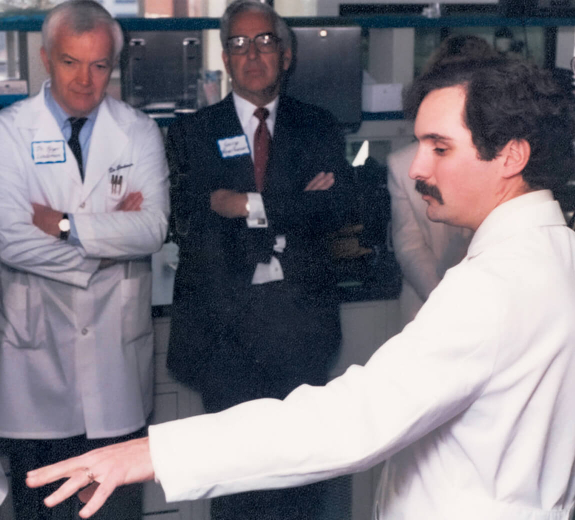
The Next Generation of BRI Researchers: Why Study T1D?
Christine Bender, PhD, Postdoctoral Researcher: “Type 1 runs in my family and seeing how they suffered really impacted me,” says Dr. Bender, whose research focuses on prevention and treatments for T1D. “It’s such an exciting time in T1D research. We have better approaches, better equipment, we’re making progress toward delaying the disease. That’s what motivates me every day.”
Noah Biru, Former Lab Aide, Current PhD candidate at Yale
“Seeing my mom struggle with managing type 1 made me want to help find a cure,” says Noah, who also lives with T1D. “BRI has opened my eyes to how interconnected the immune system is. I’m interested in studying how and why autoimmune diseases develop and persist. And I’ll always have an interest in T1D — we’re going to cure diabetes, that’s the dream.”
Lauren Knabe, Summer Intern: “At the beginning of my internship, they gave me an immunology textbook and I found every chapter to be super interesting,” Lauren says. “This research is fascinating because the immune system is this really complex puzzle that you really have to push yourself towards understanding.”