But checkpoint inhibitors don’t work for everyone — sometimes the wolf costume is just too good. And sometimes people develop side effects that look a lot like type 1 diabetes, overactive thyroid or other autoimmune diseases.
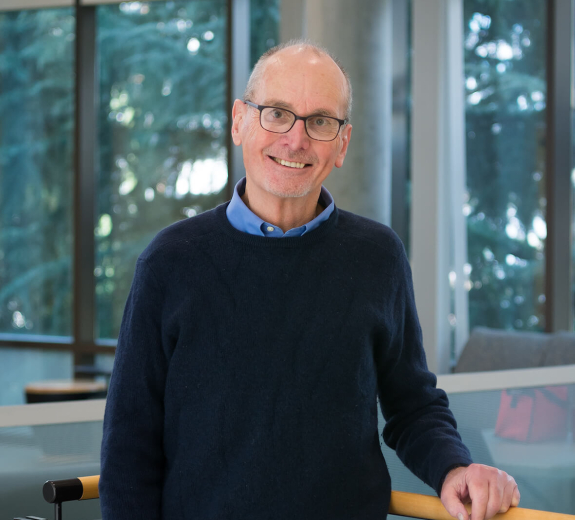
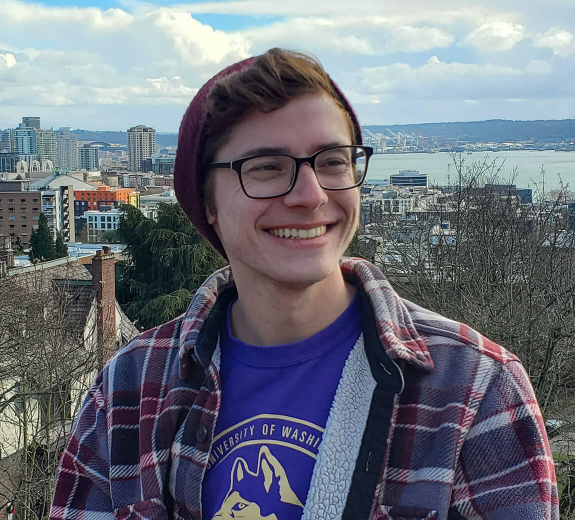
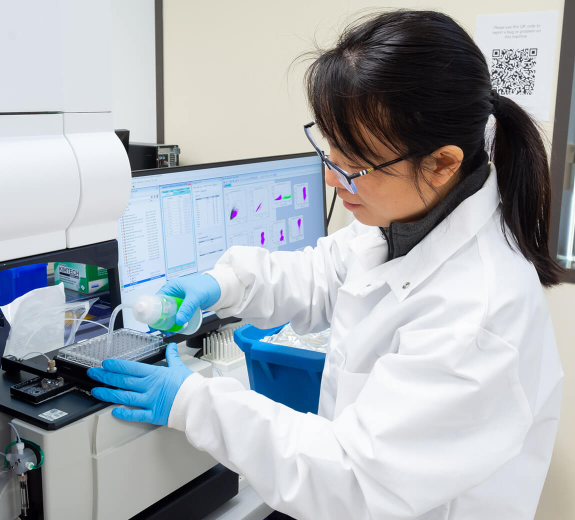
BRI scientists knew that they had the team, the tools and immune system expertise to get to the bottom of this. Now, scientists from the Linsley Lab, Buckner Lab and Long Lab are working to learn who benefits from checkpoint inhibitor therapy and how autoimmune disease-like side effects develop.
“We hope to find specific biomarkers that could predict who would respond to the therapy and who would develop autoimmune disease — and to understand if one is necessary for the other,” says BRI’s Peter Linsley, PhD.