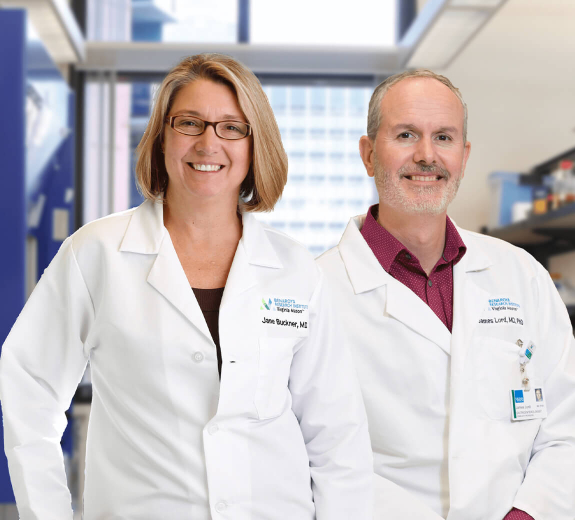
We’re all hearing that people with underlying conditions and immune deficiencies are more susceptible to COVID-19. It’s natural for people with autoimmune disease to wonder what this means for them. We sat down with two physician-researchers from Benaroya Research Institute — President Jane Buckner, MD and Principal Investigator James Lord, MD, PhD. — to get their input on some of the most common questions that people with autoimmune disease are asking about COVID-19:
COVID-19 / Coronavirus: 14 Things People with Autoimmune Disease Should Know
1. Does having an autoimmune disease increase my risk of getting COVID-19?
There is no clear connection so far between autoimmunity and COVID-19. Autoimmunity is different from immunodeficiency (in which the immune system is too weak to fight off infections). If anything, autoimmunity makes the immune system relatively over-active, often causing it to attack the body. That doesn’t mean an autoimmune patient is necessarily better at fighting infections. An over-active immune system could help fight off the virus, but it also could cause unneeded inflammation.
2. Do immunosuppressants / Prednisone increase my risk of getting COVID-19?
In most cases, it is better to stay on your medications to avoid a flare of your autoimmune disease. You should contact your doctor if you have concerns and before you make any changes in your medications.
We do not have a lot of information about immunosuppressants specifically in relation to COVID-19. But we do know that prednisone, in particular, is a major risk factor for many other infections — especially if your total daily dose exceeds 20 milligrams. This is true for all the “systemic steroids” (the ones that get into the blood and spread throughout the body), but not really a concern for steroids that are locally delivered. These local steroids include steroid skin creams (for rashes), steroid inhalers (for asthma), budesonide pills like Entocort or Uceris, and steroid suppositories or enemas for inflammatory bowel disease (IBD).
Because taking Prednisone or other systemic steroids for months makes your body critically dependent upon them, you cannot rapidly stop them or you will get quite sick. If you have been taking Prednisone for more than a month, you should ask your doctor for specific instructions if you need to taper off the medication rather than try to just go “cold turkey” on your own.
Other medications, such as methotrexate, azathioprine, mercaptopurine, and a class of drugs known as JAK inhibitors do suppress your body’s ability to fight viruses, and might make viral infections longer and more severe — but the effect is more modest than with steroids.
The new "biologic" drugs (recombinant proteins that require a shot or IV) are much more targeted and show different effects on infection. We know that anti-TNF agents (including infliximab, etanercept, adalimumab, golimumab and certolizumab , which are sold under the brand names Remicade, Inflectra, Renflexis, Enbrel, Humira, Simponi and Cimzia) increase the annual risk of a serious infection by about 1%, including influenza, a virus with similar symptoms to COVID-19. However, the impact of each type of biologic on COVID-19 may differ. In fact, one biologic drug (tocilizumab, which is sold as Actemra) is actually being studied as a treatment for severe cases of COVID-19.
3. People with “compromised immune systems” are at higher risk for COVID-19. What does that mean? Do I have a compromised immune system?
There are a variety of reasons someone might have a compromised immune system. Here’s what we know.
As stated above, certain drugs used to treat autoimmunity and chronic inflammatory conditions can compromise the immune system. There are also diseases like HIV and inborn immunodeficiencies (common variable immunodeficiency, severe combined immunodeficiency) that can severely compromise the immune system. Conventional cancer chemotherapy and radiation severely impair the immune system, especially if someone recently had a stem cell transplant. Likewise, the anti-rejection drugs used to treat people with solid organ transplants severely compromise the immune system.
More commonly, old age makes the immune system comparatively weak, but this varies a lot from person to person, so there is not a specific age when risk suddenly shoots up. We just know that older people are more vulnerable to infections in general and COVID-19 specifically.
Pregnancy is also thought of as an immunosuppressed state. That’s because a mother's immune system has to be tamped down so it accepts the father’s genes, which are in the baby and might be interpreted as being foreign agents that need to be attacked. However, at this point we do not know if pregnant women are at higher risk for COVID-19. A study done in China showed a good outcome for women infected in their last trimester, but this was a small study and does not address the impact of COVID-19 at earlier stages of pregnancy. As is always the case in pregnancy, we recommend being conservative and taking precautions to avoid contact with infected people.
4. Can hydroxychloroquine help with COVID-19? What if I already take hydroxychloroquine for lupus or rheumatoid arthritis?
Hydroxychloroquine is a medication that rheumatologists prescribe to treat a number ofautoimmune conditions, such as rheumatoid arthritis and systemic lupus erythematosus (lupus). Despite early hope that it would help fight the pandemic, studies now show that hydroxychloroquine is not necessarily effective in treating the new coronavirus. People who are taking this medication for a disease such as lupus or RA should continue using the medication. Learn more about hydroxychloroquine in the time of COVID-19.
5. Is there any data on how the coronavirus affects people with autoimmune disease?
Since this is such a new virus, we do not have information on how it impacts people with autoimmune disease. BRI’s team is currently planning research on this and we will know more in the coming weeks and months as physicians and scientists around the world collect data. We are all working toward the goal of understanding how to predict who is at highest risk and how to protect them.
6. I have an autoimmune disease. Should I cancel my doctor’s appointments?
That depends on why you need to see your doctor. Many clinics are offering remote services like telehealth for routine visits. That said, your doctor may want to see you in person, particularly if you have a new or very active health problem.
At this time when hospitals and physicians are busy with the care of COVID-19 patients, it makes sense to contact your clinic in advance to find out if they recommend that you come to your appointment or if they could postpone it or make it virtual.
7. I have an autoimmune disease. Is it safe for me to leave the house?
The answer to this seems to change by the day and it’s important to listen to your local officials. You should retain social distance when you leave your home and to make sure you clean your hands after touching objects that may have been handled by other people. This is important not only for your health but also for the sake of everyone in our society. Our goal is to limit the spread of the infection and we all have a role in doing that.
8. What supply of prescription medication should I keep on hand (e.g. in case of quarantine)? What do you advise for people who receive infusions?
The CDC is recommending a 30-day supply of self-administered drugs. We are still advising that people who must get their medication administered by a facility (like IV meds) come in on-schedule for each dose (unless they feel symptoms of COVID-19). Some insurance plans allow home infusions as an alternative to infusions in a facility, but it is unclear if this increases or decreases infection risk, as traveling infusion nurses and their equipment visit many households, some of which may be much higher risk than an infusion center.
9. What should my immediate family do to protect me / should they self-quarantine?
Anyone who is entering and exiting your house on a regular basis must practice good protective hygiene:
- Wash hands for at least 20 seconds with soap and water when they arrive at your home
- Stay six feet away from others in public
- Use a barrier (like an antibacterial wipe) to touch common surfaces like door and sink handle
- Avoid touching their own faces
Likewise, anyone in your home with a fever and/or other COVID-19 symptoms should be isolated as much as possible. As shopping in actual stores has largely been replaced with mail-order, it is also not a bad idea to wash hands after retrieving and opening mail.
8. I have an autoimmune disease. Should I cancel my doctor’s appointments? Is it safe to go to a blood draw?
That depends on why you need to see your doctor. Many clinics are offering remote services like telehealth for routine visits. That said, your doctor may want to see you in person, particularly if you have a new or very active health problem.
If you do need to go to an appointment or blood draw in person, we recommend the same sorts of precautions that are being recommended for any outing:
- Wear a mask and perhaps disposable gloves
- Wash or sanitize hands (or gloves) frequently
- Keep your hands away from your face as much as possible
- Use elbows and wrists when possible to open doors, push elevator buttons, etc.
- If you have a fever or bad cough, stay home — lab work can probably wait until you feel better.
There are also services that send visiting nurses to your home for a blood draw. If this isn’t convenient or if you don’t feel comfortable, don’t worry — visiting a clinic for a blood draw is just as safe, if not safer, than an outside nurse coming to your home.
9. I'm hesitant to contact my doctor right now because they’re so busy with COVID-19. Is it OK to contact my doctor if my symptoms change, even if the change is minor?
Your threshold for contacting your doctor for health care should be no different now than it ever was. In fact, in response to the pandemic, virtual appointments are more accessible than ever. It may actually be unusually easy (and safe) to contact your doctor now.
Despite early concerns that healthcare professionals would be overwhelmed by the pandemic, this did not really happen in the United States outside of New York, and many specialties are now actually quite underutilized. Thus, unless your regular doctor is an infectious disease specialist or works in an intensive care unit, they probably have plenty of time to hear from you and help you.
10. What supply of prescription medication should I keep on hand (e.g. in case of quarantine)? What do you advise for people who receive infusions?
CDC is recommending a 30-day supply of self-administered drugs. We are still advising that people who must get their medication administered by a facility (like IV meds) come in on-schedule for each dose (unless they feel symptoms of COVID-19). Some insurance plans allow home infusions as an alternative to infusions in a facility, but it is unclear if this increases or decreases infection risk, as traveling infusion nurses and their equipment visit many households, some of which may be much higher risk than an infusion center.
11. I’m getting medication shipped to me. How do I sanitize the box and ensure mail doesn’t bring germs into my home?
First, viruses don't generally survive for very long outside of the body, so if the mail or its contents have not been in contact with people for many days, there are probably not a lot of viable germs.
The highest risk is likely to be the external packaging, as that will have been in contact with people the most recently — but packages should not be able to aerosolize particles to cause a lung infection. Therefore, if you remove and discard the external packaging of your mail, and then wash your hands, you should be at pretty low risk. If you are really worried, you could expose your mail to a UV light for an hour before handling it or wipe it with bleach or alcohol.
12. I’m feeling stressed and having trouble sleeping. What can I do?
Practice "good sleep hygiene." Be very consistent, going to sleep at the same time every night and waking up at the same time every morning, not more than an hour or two after dawn at the latest. Set an alarm if you need it to maintain this consistency, even if you don't have a schedule that requires it. Some other tips include:
- Sleep while it's dark and be awake while it's light. Consequently, try to avoid napping during the day, even if you are really tired from having gotten so little sleep the night before. Save that precious sleepiness for the evening.
- Reduce caffeine intake. Combating daytime fatigue with stimulants, like caffeine, will only make it harder to sleep at night. Limit any caffeine consumption to the morning.
- Train your body that your bed is only for sleeping. Do not lie in bed to read or watch TV. In fact, if you toss and turn in bed trying unsuccessfully to fall asleep (or back to sleep), you should give up after about half an hour, get out of bed, and spend at least 15 minutes doing something else, like reading a book in another room, before going back to bed and trying to fall asleep again.
- Avoid alcohol. It’s a terrible sleep aid. It usually only makes a person sleepy for the first hour or so after blood alcohol initially rises, and then paradoxically either makes it harder to sleep or makes sleep very shallow and low quality thereafter, resulting in increased fatigue the next day.
Read more: Tips for Living with Autoimmune Disease During COVID-19: Managing Stress and Building Resilience
13. How can I keep my immune system as strong as possible?
Most products that claim to “strengthen the immune system” do no such thing (particularly those promoted by unregulated, for-profit vitamin manufacturers), but you can certainly avoid things that would weaken it. Staying up late and getting too little sleep, or having a very erratic sleep schedule, makes the immune system weaker. Try to get to bed and wake up regularly, sleeping at night and being awake in daylight.
If you smoke, quit now. Smoking might weaken the immune system but definitely weakens the lungs, and is a clear risk factor for death in COVID-19. Similarly, marijuana use, especially smoked, is probably not helpful. Other illicit drugs and alcohol may or may not impair immunity, but they definitely impair judgement, and given how careful we now need to be, being impaired may itself be a bigger risk factor for COVID-19 than anything involving the immune system.
14. How can I stay active and healthy while I’m at home?
Jogging or walking alone has generally not been forbidden, but you certainly should keep your distance from others and stay inside if you are sick or unusually vulnerable. If you have a home with stairs, consider putting things you use regularly on different floor to force you to walk up and down many times a day. Floor exercises (sit-ups, push-ups etc.) are something that require no equipment, just willpower. A lot of exercise videos on streaming platforms have replaced group workouts and can be followed at home. Track your exercise in a journal to see if you can make improvements.
If you live in a complex with a shared gym, do NOT use it. Gym equipment surfaces are high risk for contamination.
Probably even more important than exercise is to avoid using food as entertainment. People eat when they’re bored, which means they gain weight. Weight gain has been associated with diabetes, and diabetes is another clear risk factor for severe effects in COVID-19. If you have diet-controlled diabetes or have been told that you have “metabolic syndrome,” you should be particularly vigilant about what you eat while in isolation.
Part of the challenge is that fresh fruits and vegetables do not last, so our diets may move more towards carbohydrates and preserved or frozen foods, since we’re not going to grocery stores as often. Frozen vegetables, while not as great (or great-tasting) as fresh, are better than no vegetables, so stock up on these if you have the freezer space, and make them a central part of your meals. Avoid snacking between meals. If that’s too hard, try to snack on a plant. Carrots, apples, pickles, and dried fruits keep a long time without freezing, and are convenient to snack on without any prep time. What you do not want to do is open a bag of chips or a tub of ice cream in front of the TV. Before you know it, you will have eaten the whole container.
Also, be careful with alcohol and other inebriants as a solution to boredom. It surprisingly easy to hurt your liver with alcohol when it is consumed on a daily basis for an extended period of time. If you were a weekend drinker before the pandemic, do not start treating every day as a weekend just because you are no longer going to work in person.
Finally, maintain your psychological health. Try to stick to old patterns. If you used to set your alarm to go to work, keep doing it — don’t sleep in just because you can. Keep showering and grooming even though nobody new is going to see you. Get dressed every day, maybe even in your usual work clothes.
If you are telecommuting, do it while sitting in a dedicated work space that won’t hurt your body. Maintain a consistent work schedule, with a specific time for lunch. Work a normal length day, if you can. If it is allowed and you are well, take a walk, a bike ride or a drive at least once a day.
Immuno-what? Hear the latest from BRI
Keep up to date on our latest research, new clinical trials and exciting publications.