A New Cell with Global Implications
When people with diseases like lupus and systemic juvenile idiopathic arthritis (SJIA) are feverish and light-headed, doctors start to worry: These symptoms can indicate a life threatening condition called macrophage activation syndrome (MAS).
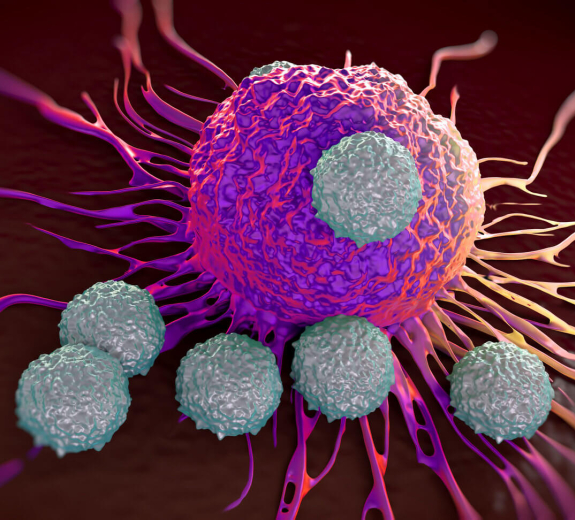
MAS strikes when macrophage cells – which should eat bacteria – eat red blood cells instead. BRI principal investigator Jessica Hamerman, PhD, and postdoctoral fellow Holly Akilesh, PhD, recently discovered that a specific macrophage, which they named an “inflammatory hemophagocyte” (iHPC), is the culprit behind MAS. This could have big implications for patients with autoimmune diseases – and even for kids with malaria.
“If we can figure out how to get rid of iHPCs or keep them from eating healthy red blood cells, we might prevent MAS,” Dr. Hamerman says.
Key Protein Changes
“Now that we know how this unusual cell develops, we can work toward new ways to treat and prevent MAS,” Dr. Hamerman says.
Help for Kids with Malaria
Dr. Hamerman was curious if iHPCs play a role in MAS-like anemias in people with conditions besides autoimmune diseases. She decided to study malaria because it often leads to severe malarial anemia page3 (SMA) – the second leading cause of death for kids with malaria.
Dr. Hamerman partnered with University of Washington malaria expert Marion Pepper, PhD, to study how SMA starts. Their findings weren’t just similar to those in the autoimmune disease study. They were identical.
“The exact same pathway and the exact same cells play a significant role in SMA,” Dr. Hamerman says. “So if we can develop therapies that prevent severe anemias in patients with autoimmune diseases, they might work for kids with malaria.”
Goal: Real-World Treatments
Now Dr. Hamerman and her team are moving toward real-world clinical applications.
This includes partnering with Seattle Children’s Hospital rheumatologist Susan Shenoi, MD, to collect samples from kids with MAS. The team plans to use those samples to investigate ways to inhibit the iHPC cells that cause MAS.
“We’re very excited about Dr. Hamerman’s work because knowing more about what causes MAS will help us develop better, more targeted medicine,” Dr. Shenoi says.
Dr. Hamerman is also working with the NIH’s Peter Crompton, MD, MPH, to study samples from malaria patients.
“Thanks to many collaborators at BRI and beyond, we’ve started moving our findings from the lab to the clinic to hopefully help people around the world,” Dr. Hamerman says.
Immuno-what? Hear the latest from BRI
Keep up to date on our latest research, new clinical trials and exciting publications.


