Discovery of a Commonality in Autoimmune Disease
Benaroya Research Institute is committed to fighting the more than 80 autoimmune diseases. Because autoimmune diseases all share a common cause—mistakes made by the body’s immune system—scientists can use breakthroughs made against one autoimmune disease to make progress against them all.
BRI scientists are now discovering a new, exciting commonality between autoimmune diseases. This research points to an early event that drives the development of autoimmunity and which could be targeted by new therapies. They are pioneering research into this critical driver of autoimmune diseases that is present in rheumatoid arthritis, type 1 diabetes, celiac disease and most likely multiple sclerosis. Their investigation focuses on proteins that are modified when the body experiences environmental stresses. Generally, the immune system has a system of checks and balances so it can protect the body against infections without overacting, but certain stresses can disrupt that balance.
Modified Proteins
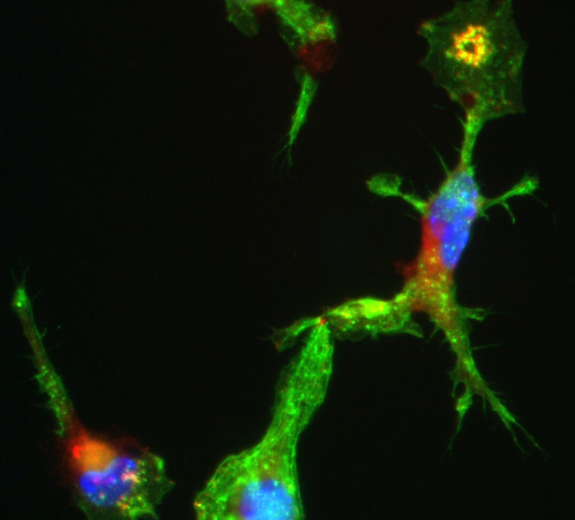
“We have found that when the body undergoes stresses such as a viral infection, it increases enzymes in the body that modify or alter its own proteins. These modified proteins can activate T cells to mistakenly attack and destroy healthy cells in the body, causing autoimmune disease,” says Eddie James, PhD, who is conducting a number of studies regarding T cell responses toward these proteins.
In 2014, BRI President Jane Buckner, MD, and Dr. James identified T cells that react to such modified proteins in the joints of people with rheumatoid arthritis (RA). They were able to demonstrate that the number of these T cells was increased in the blood of people with RA but that they were reduced with immune modulating treatments. Dr. James later demonstrated that similar T cells are present in people with type 1 diabetes and hopes to extend this research into other autoimmune diseases such as multiple sclerosis.
New Area of Collaboration
These discoveries open up a whole new area of research, and Dr. James is now collaborating with many other groups to study the recognition of modified proteins. These include:
University of Colorado and Karolinska Institutet, Sweden—Drs. Buckner and James are collaborating with these institutions to see how the altered proteins affect people with RA. For instance, they plan to look at family members who are at high risk for developing RA and to perform studies to determine whether effective therapies eliminate these T cells. This collaborative work will also include structural studies to investigate why modified proteins are so effective at activating T cells.
University of Pittsburgh—Dr. James is working with Jon Piganelli, PhD, to see how the altered proteins affect type 1 diabetes (T1D). In T1D, the immune system mistakenly attacks beta cells in the pancreas. Beta cells create insulin that the body needs to live. “Beta cells may be the most stressed cells in the immune system,” says Dr. James. “Every time you eat, the beta cells have to release insulin and then restock. The stress can alter proteins in a way that causes T1D. Our collaborators have developed some anti-stress molecules. We want to see whether treating beta cells to block these stress pathways has the potential to slow down the disease process.”
Yale University—Dr. James is collaborating with Mark Mamula, PhD, to see if there are new biomarkers that can measure responses to modified proteins in type 1 diabetes. These studies would help further define at-risk family members who should be considered for prevention studies.
Immuno-what? Hear the latest from BRI
Keep up to date on our latest research, new clinical trials and exciting publications.


