3. How do virus variants happen?
Virus variants happen when a virus reproduces and spreads. Viruses spread by making copies of themselves and their genetic code. But sometimes when they make those copies, they make typos called “mutations.”
“Virus variants happen in the same way humans evolved from Neanderthals — when we reproduce, we see these tiny changes in genetic code,” Dr. Lacy-Hulbert says. “Sometimes those changes help us survive, like having thumbs or walking upright. Individuals with those mutations survive better, reproduce, and pass on those genetic traits.”
The more the virus spreads, the more opportunities it has to reproduce and change. That’s how new variants arise.
“Every time that the virus gets copied, a few little errors might creep in,” Dr. Lacy-Hulbert says. “That means that every time it goes through an infection, you might get a slightly different version of the virus coming out of each cell. And when one of those versions has an advantage over another — say it’s more contagious — that variant lives on.”
4. What is the delta variant?
The delta variant is one of four COVID-19 variants being monitored in the United States as of publication in August 2021. It was first identified in India in December 2020 and first found in the United States in March 2021. This variant appears to spread more quickly and easily than other variants.
5. Is the Delta variant more contagious? Is the delta variant more dangerous?
The Delta variant has some mutations in the genetic code that make it more contagious than the earlier variants. People who test positive for the Delta variant have more virus particles in their airways, which makes it spread more easily.
“We’ve yet to see any convincing data that Delta is a lot more deadly — that it's making people a lot sicker,” Dr. Lacy-Hulbert says. “It's definitely more contagious which is probably why there are so many hospitalizations and severe cases right now.”
6. Are current vaccines effective against variants? Are scientists making vaccines to target variants?
The vaccines are effective against current variants of COVID-19. The vast majority of people experiencing severe disease are unvaccinated. It's still possible for vaccinated people to get infected, but vaccines dramatically reduce the risk of serious illness that leads to hospitalization or death.
Scientists are also actively conducting research to create vaccines specifically targeted to COVID-19 variants.
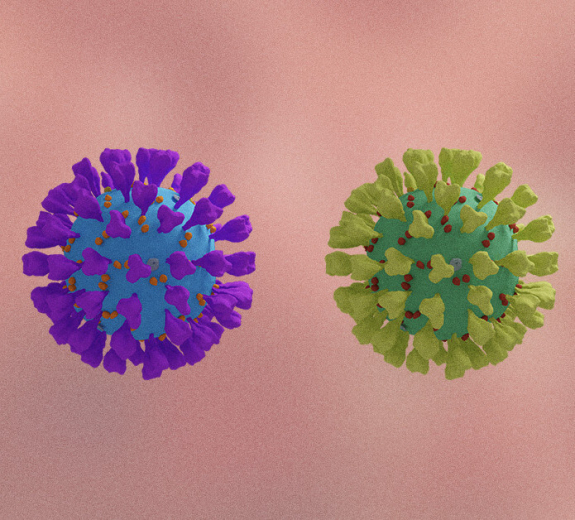
7. Could COVID-19 mutate to evade vaccines?
Current vaccines target a key part of the virus called a spike protein, which allows the virus to enter your cells. The vaccines are a little less effective at preventing infection by some variants which have mutations in the spike protein. However, so far there are no variants that completely evade the vaccines.
“The vaccine targets an interaction that’s essential for the virus to infect your cells and spread through your body,” Dr. Lacy-Hulbert says. “Mutations can make vaccines slightly less effective. But it would be very difficult for the virus to mutate enough to evade the vaccine’s protection entirely.”
8. What is a breakthrough COVID-19 case? Why are there breakthrough cases of COVID-19?
A breakthrough case happens when someone tests positive for COVID-19 even though they’ve been vaccinated. Most people who experience breakthrough COVID-19 cases have mild illness and some have no symptoms at all.
“The vaccine is very good at stopping COVID-19 from spreading through your body and getting severe symptoms, but it doesn’t stop the virus from getting into your nose and lungs,” Dr. Lacy-Hulbert says. “When we test for COVID-19, we’re testing whether there’s any virus in your airway. When we hear about breakthrough infections, we’re often talking about people who have the virus in their airways and test positive, but these are not typically people who are getting really sick.”