“For the first time, BRI researchers have identified and are able to target a unique type of cell that causes allergies. Up until now, we couldn’t easily identify the ‘bad guy’ cells triggering allergies from the ‘good guy’ cells protecting the body,” says Steven Ziegler, PhD, who leads BRI’s Immunology Research Program. “This makes allergy research much more straightforward and opens the door to therapies that could target this common enemy and transform treatment.”
Allergies affect 25 percent of the population or 50 million people in the U.S., and the incidence is increasing. It is estimated that by 2050 about one in two people will have allergies. Allergies occurwhen the body’s immune system makes a mistake and overreacts to a foreign substance (an allergen), such as pollen or animal dander, that in most people is generally harmless. Allergies can range from mild to severe. For some people, they can compromise quality of life and even be life-threatening.
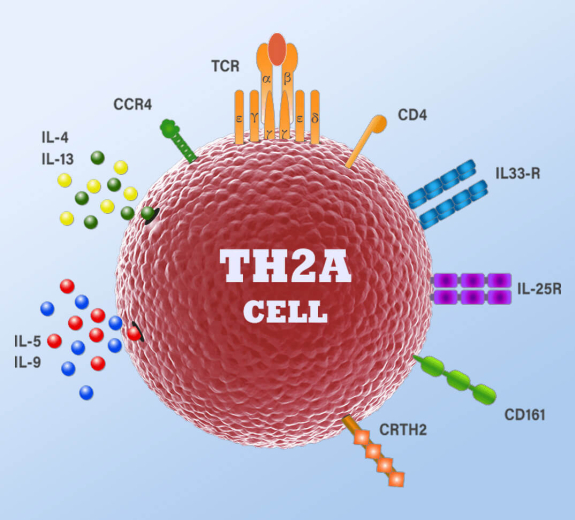
BRI’s research, led by Dr. Wambre, began seven years ago, by examining a type of immune cell, called a Th2 cell, that helps orchestrate how the immune system responds to parasites, viruses and bacterial infections but also leads to allergies.
As Dr. Wambre and his colleagues analyzed human blood samples containing these cells, they discovered a specialized subtype of cell, which they called Th2A, that is present in people with allergies but almost entirely absent from people who don’t have allergies. They performed tests to confirm that Th2A cells play a pivotal role in at least six common allergies—including peanut, grass pollen, mold, cat dander, dust mite and tree pollen.
The research team also analyzed Th2A cells in blood samples from participants in a clinical trial of a new therapy for peanut allergies. Dr. Wambre and his colleagues found that the Th2A cells were activated when participants were exposed to the peanut allergen or an environmental pollen. Also the number of Th2A cells decreased as participants became desensitized to the peanut allergen during the study.
“This is the first time we’ve had a way to accurately measure the allergy process and assess whether therapies are working,” says Dr. Wambre. Even more important, researchers can now pursue therapies that potentially disarm Th2A cells and stop allergies.
The study’s results have already caught the attention of leading allergy research and advocacy organizations including Food Allergy Research & Education (FARE), which awarded Dr. Wambre a five-year Mid-Career Investigator Award in 2015.
“This could make allergy research much more directed, since scientists can now focus on the specific cells involved in generating allergies,” says James R. Baker Jr., CEO and chief medical officer of FARE, which funds research on new allergy therapies. “We’re hopeful that studying Th2A cells will quickly improve our understanding of how allergies develop and lead to therapeutic approaches to block allergies. This would improve the lives of allergy sufferers tremendously.” BRI and Virginia Mason are members of the FARE Clinical Network Centers of Excellence.
A strong collaboration between Wambre’s laboratory, BRI’s Translational Research Program including the biorepository team, allergy research participants and Virginia Mason’s Drs. Jeong, Robinson and Farrington helped to make this discovery possible.
BRI studies diseases caused by imbalances of the immune system, including autoimmune diseases, allergies and asthma, among others. Autoimmune diseases occur when the immune system mistakenly attacks its own healthy tissues. Allergies and asthma occur when the body’s immune system overreacts to substances that are generally considered harmless. When BRI scientists were studying the immune system in autoimmune diseases, they discovered significant cells and mechanisms that pertained to allergies and asthma. They continue to pursue these areas in efforts to rebalance the immune system and improve human health.